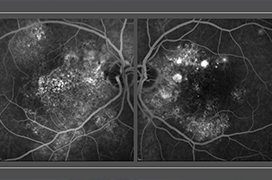
Central serous chorioretinopathy (CSC) is a disease characterized by serous detachment of the neuroretina, especially in the posterior pole of the eye. It is often accompanied by serous detachment of the retinal pigment epithelium (RPE) and associated with the leakage of fluid into the subretinal space through the defective RPE. CSC most often affects men of working age. The exact pathophysiology of the disease is not completely known. Based on indocyanine green angiography (ICG), which revealed increased permeability of choroidal vessels, and optical coherence tomography (OCT) showing increased choroidal thickness, choroidal vasculopathy is assumed to be the primary cause of CSC. In most cases, CSC has a good prognosis with spontaneous resorption of the subretinal fluid (SRF) and improvement of visual functions. However, in a small percentage of patients the disease progresses to a chronic or recurrent course, and can lead to irreversible functional and anatomical changes of the retina with a final clinical picture of diffuse retinal pigment epitheliopathy (DRPE). The optimal treatment approach for patients with CSC remains controversial. In recent decades, myriad therapeutic approaches have been used in the treatment of chronic forms of CSC (cCSC); these included for example laser photocoagulation, pharmaceutical treatment, standard photodynamic therapy (PDT) or anti-VEGF. In recent years a less destructive method, specifically PDT in reduced dose regimens, either with a reduced dose of verteporfin or the laser beam energy used, has been preferred in the treatment of cCSC. Comparable efficacy and safety has been demonstrated using reduced-dose or reduced-fluence PDT regimens in patients with cCSC, with an improvement in best-corrected visual acuity and reduction of SRF.
- Central Serous Chorioretinopathy. A Review
- Diagnostic Challenges of Ocular Rosacea
- Multimodal Imaging of Choroidal Nodules in Neurofibromatosis Type I
- Comparison of Early Vision Quality of Sbl-2 and SBL-3 Segmented Refractive Lens
- The Impact of the Covid-19 Pandemic on The Quality of Examinationi Eye Clinics in the Czech Republic – Questionnaire Study
- Kaposi’s Sarcoma. A Case Report